شن و ماسه چین ساخت معدن سنگ
محجر الجرانيت في التعدين هوسور-شن و ماسه چین ساخت معدن سنگ
689
مجموعات (مجموعات)
مع أكثر من 30 عامًا من الابتكار والتطوير ، أصبحت شركة تتمتع بقوة كل من الأجهزة والبرامج في صناعة آلات التعدين المحلية
120㎡
COVER
أنشأت الشركة مجمعات صناعية تغطي مساحة 120 متر مربع ، وأنشأت مكاتب في روسيا وكازاخستان وإندونيسيا وأماكن أخرى.
170+
الدول المصدرة
لقد حصلت جميع المنتجات على شهادة نظام الجودة الدولية ISO9001: 2008 ، وشهادة الاتحاد الأوروبي CE وشهادة الجودة الروسية GOST ، وقد نجحت في التغلب على أكثر من 20000 عميل في أكثر من 130 دولة ومنطقة حول العالم.
مشروع
مرحبا هل يمكنني مساعدتك؟
محطة تكسير الصخور 150 طن في الساعة في إيركوتسك ، روسيا
السعة: 10-80 طن / ساعة
حجم منتجات إينال: 0-5-20-40mm
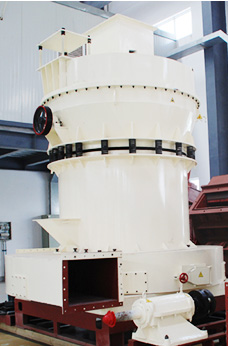
المعدات: MTW EUROPEAN TYPE TRAPEZIUM MILL + Vibrating Screen + حزام ناقل + جهاز تغذية بالاهتزاز
- البحرين في مخروط محطم
- اندونيسيا معدات تعدين خام الحديد
- فروشنده سنگ شکن موبایل سنگ طلا کوچک در فیلیپین
- كسارة الفك الجرانيت مصر
- جزئیات فرآیند آسیاب ریموند
- الفك كسارة الحجر كسارة حجر الفك محطم آلة
- كسارات للبيع منجم للذهب في الولايات المتحدة الأمريكية غانا
- اخر اختراع ماكينات
- للب تهتز الشاشة الهند
- مشروع محلي الصنع aeee
- آلة الحفر شعار عينة
- كوريا بارا لا فينتا دي تريتورادورا دي بيدرا إن وي
- معارض المعدات الثقيلة في أربيل
- نموذج لإنتاج كسارة الزجاج
- للحجر صغير سحق تصميم
- ماشین خرد کن 500
- استخدمت كسارة في أوروبا دراسة جدوى قبل
- سنگ شکن ضربه ای انتظار کاهش سنگ شکن موبایل
- عوائق آلة الطحن
- دوارة طبل المحبب المصنعة في الفلبين
- تفسير مكن وضو انبي محمد
- آلة لسحق الصخور إلى مسحوق
- المحمول المتعاقدين إعادة تدوير الخرسانة في إلينوي
- كسارة مخروط الرسم
- مبدأ عمل طاحونة بكرة رأسية
- طواحين اسمنت اسيوط سيمكس
- طواحين حجرالجبس
- عيب على القوائم inrolling حالة مطاحن العملاء
- فولاد ضد زنگ را فشار دهید شراب
- الاسمنت ريمون أجزاء مطحنة المورد الدول موحدة كسارات الحجر
- تاريخ المحاجر والتعدين في akamkpa
- كيفية بناء مطحن
- وكم تكلفة كسارة الصخور 145
- آرد ارزن تصویر الک
- كسارة حجر للبيع في راجستان
- الحديد مصنع المحجر خام للبيع في المكسيك
- النقلات الممنوعة في الشطرنج
- تعطل سحق من قبل مطحنة الكرة
- tkf jaw crsher ibag eb 850
- تكلفة منبع الأسفلت
- طحن وسائل الاعلام مما أثار انفجار
- يمكن الترهل ومطحنة الكرة مطحنة لديها نفس الأبعاد
- قيادي مصنع لتجهيز الزنك للبيع جنوب أفريقيا
- ما هي المعدات المستخدمة من قبل التعدين
- عملية كسارة الرمال القصدير